What is Osteoporosis?
Osteoporosis, meaning porous bone, is a disease in which the density and the quality of the bone is reduced. Bone is living tissue that is constantly being broken down and rebuilt. Osteoporosis occurs when the creation of new bone does not keep up with the loss of old bone. As bones become more porous and fragile, the risk of fracture is greatly increased, even with minimal to no trauma. There are 1.5 million osteoporotic fractures in the United States every year. Fractures may cause a loss of independence, chronic pain, disability, and even death.
Monument Health’s team of board-certified specialists have extensive expertise in diagnosing and treating osteoporosis. Our team has multiple specialists involved in the care of osteoporosis, including rheumatologists, endocrinologists, orthopedic surgeons, internal medicine physicians, family medicine physicians, physical and occupational therapists.
Our comprehensive program offers the latest diagnostic tests available, including a DXA scan. This bone density test uses special x-rays to diagnose osteoporosis and to follow your treatment. Monument Health performs over 2000 DXA scans a year and has some of the newest technology available to perform DXA scans.
The treatment of osteoporosis often involves medications that can be pills, injections or infusions. Monument Health nurses have extensive experience in preauthorization for insurance and administration of medicines.
We will work with you to develop a personalized treatment plan for your unique needs.
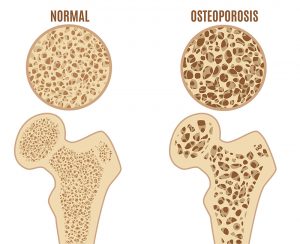
The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs. Because osteoporosis usually develops without any symptoms, it is important to get screened. It is estimated that a 50-year-old female has a 40-50% chance of an osteoporotic fracture in her remaining lifetime. Any kind of fracture may occur, but the most common are fractures of the spine, hip, and wrist. Osteoporosis does not have to be an inevitable part of aging; it’s a disease that can be prevented and treated.
Patient Education
Risk factors
A number of factors can increase the likelihood that you will develop osteoporosis, including age, race, lifestyle choices, and medical conditions and treatments. Some risk factors are unchangeable, but some can be modified.
Unchangeable risk factors
Sex: Females are much more likely than males to develop osteoporosis.
Age: The older you get, the greater your risk for osteoporosis, especially if you are a postmenopausal female.
Race: Osteoporosis affects men and women of all races, but you are at greater risk of osteoporosis if you are of Caucasian, European or Asian.
Family history: Having a parent or sibling with osteoporosis puts you at greater risk, especially if your mother or father had a hip fracture prior to age 80.
Body frame size: Men and women who have small body frames tend to have a higher risk because they typically have a smaller bone mass.
Medical conditions: Osteoporosis risk is higher in people with certain medical conditions, including kidney or liver disease, lupus, cancer, celiac disease, inflammatory bowel disease, hyperparathyroidism and rheumatoid arthritis
Modifiable risk factors
Vitamin D deficiency: Lack of adequate vitamin D, either through diet or sun exposure, contributes to osteoporosis risk.
Dietary factors: Excessive caffeine, soda or alcohol use, or a lifetime lack of dietary calcium increase the risk of developing osteoporosis. Eating disorders in which food intake is severely restricted can increase the risk of osteoporosis.
Body weight: Having a low body weight and less muscle increases the risk of osteoporosis.
Certain medications: Taking glucocorticoids (steroids), protein pump inhibitors (PPI) use for treating acid reflux, certain cancer treatment drugs (particularly for breast or prostate cancer), excessive thyroid hormone replacement, anticonvulsants, diuretics, transplant rejection and other medications can affect bone density.
Gastrointestinal surgery: Surgery to reduce the size of your stomach or remove part of your intestines limits the amount of surface area available to absorb nutrients, including calcium and vitamin D.
Sex hormones: Lower sex hormone levels tend to weaken bone. The reduction of estrogen level in women after menopause is one of the strongest risk factors for developing osteoporosis. Treatments for breast cancer that reduce estrogen levels in women are likely to accelerate bone loss. Men have a gradual reduction in testosterone levels as they age, and treatments for prostate cancer that reduce testosterone levels are likely to accelerate bone loss.
Thyroid problems: Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive or if you take too much thyroid hormone medication to treat an underactive thyroid.
Lifestyle choices
Smoking: Tobacco use contributes to lower bone density.
Excessive alcohol consumption: Regular consumption of more than two alcoholic drinks a day increases your risk of osteoporosis.
Sedimentary lifestyle: Lack of physical activity contributes to low bone density.
Criteria used for diagnosis of osteoporosis
Osteoporosis can be diagnosed by three criteria in the United States:
1) T-score of -2.5 or lower on a DXA scan (World Health Organization criteria)
2) T-score between -1 to -2.5 on a DXA with a high FRAX score
3) A fragility (low trauma) fracture after the age of 50
A T-score represents the number of standard deviations that your DXA results are different from a health 30-year-old of the same sex.
A FRAX score is your risk of having an osteoporosis-related fracture in the next 10 years. The FRAX score is calculated using questions about age, sex, height, weight, previous fracture, parental hip fracture, current smoking, glucocorticoids (steroids), rheumatoid arthritis, greater than two drinks of alcohol per day, and your femoral neck bone mineral density from the DXA test.
A Fragility (low trauma) fracture is any fracture that occurs with little to no trauma. A fall from standing height that results in a fracture is considered to be a fragility fracture.
Calcium Questions
How much calcium do I need? The National Osteoporosis Foundation recommends 1200 to 1500 mg of calcium per day for all adults.
Can I take too much calcium? Yes, but it is a rare problem. If you consume very large amounts of calcium, more than 3000 to 4000 mg/day, it may increase your risk of kidney stones.
What kind of calcium is best? The best calcium is from your diet. This includes dairy products, certain green vegetables, and calcium fortified fruit juices, soy or almond beverages. If you do not receive adequate calcium in your diet, any brand name or generic calcium product that meets USP (United States Pharmacopeia) standards is probably fine. The real issue is getting enough calcium, not what kind of calcium you take.
Are there are different types of supplemental calcium: Yes, calcium carbonate is the most common and typically the cheapest supplement. The second most common supplement is calcium citrate. If you are on a medication for GERD/reflux/heartburn, you may want to take calcium citrate for better absorption. There are also multiple forms of the supplement, including pills, gummies and liquids.
How do I take the calcium? Calcium carbonate should be taken with a meal or snack. Calcium citrate can be taken with or without food. To assure maximum absorption, it is best to divide the calcium intake during the day so that you do not take any more than 500-600 mg at one time.
What do I do if calcium bothers me? If calcium carbonate upsets your stomach, switch to calcium citrate. If you have problems with constipation, try calcium citrate or a calcium that contains magnesium, which is a natural laxative.
Can I take calcium if I have had a kidney stone? Yes. Even people with kidney stones need calcium to have strong bones. Calcium citrate may be the preferred type of calcium for patients with previous stones. It is important to drink plenty of liquids to keep your urine dilute. Contact your physician if you have any special concerns.
Are there people with higher requirements than the standard recommended dose of calcium? Yes, it is not enough to just take in enough calcium every day – you must also have a functional intestinal track and adequate amount of vitamin D. If you had a Roux-en-Y gastric bypass surgery for weight management, Inflammatory bowel disease (Crohn’s or Ulcerative colitis), or Celiac disease, you may have higher requirements. Some medications can change the calcium requirements. If you have concerns, discuss them with your primary care provider.
Vitamin D questions
What is vitamin D? Vitamin D is a fat soluble vitamin that works with other vitamins, minerals and hormones to maintain normal blood levels of calcium and phosphorus. It increases the absorption of calcium from the intestines and promotes retention of calcium by the kidneys.
How much vitamin D do I need? The recommended daily intake of vitamin D varies according to age. In South Dakota and Wyoming, the requirement is approximately 1000-2000 International Units (IU)/day for an adult.
What are the consequences of not getting enough vitamin D? Vitamin D deficiency can impair calcium metabolism enough to cause osteoporosis, osteomalacia, or rickets, depending on the age and the severity of the deficiency. A condition called “secondary hyperparathyroidism” which increases the rate of bone metabolism and causes loss of bone, often occurs with vitamin D deficiency. Reduced muscle strength and increased risk of falls may also occur with vitamin D deficiencies.
How common is vitamin D deficiency? In South Dakota and Wyoming, approximately 50% of adults are vitamin D deficient if they are not taking a vitamin D supplement.
Can I get too much vitamin D? Yes, you can get too much, but vitamin D toxicity is a very rare condition that is insignificant in comparison to vitamin D deficiency.
How do I get vitamin D? In children, exposure to sun with normal outdoor activities is usually sufficient. As adults age, there is a decreased ability to produce vitamin D with sun exposure. All adults should consider taking a daily vitamin D supplement.
Are there people with higher than normal requirements for vitamin D? Yes, patients who have had gastric bypass surgery often have a much higher than normal requirement for vitamin D. The amount of vitamin D that the patient needs is easily determined with a simple blood test.
Medications for osteoporosis
Your health care provider may suggest that you take a medicine that will help your bones to become stronger and resist breaking. These medications, along with diet, exercise and healthy lifestyle choices will help your bones stay healthy and reduce the risk of a fracture. For the maximum benefit of the medication, you must be on adequate calcium and vitamin D. Bone is living tissue that is constantly being remodeled, and different medications work at different points of the remodeling process. Medications are approved for use when there is strong evidence that the benefit of treatment outweighs the potential risks of side effects.
Bisphosphonates: Medications that reduce bone breakdown (resorption) and allow strong new bone to be created by your body include:
- Alendronate (Fosamax)
- Ibandronate (Boniva)
- Risedronate (Actonel)
- Andzoledronic acid (Reclast)
How to take the tablets: Take first thing in the morning on an empty stomach with 6 to 8 ounces of plain water, 30 minutes before eating or taking other medications or drinking anything other than water, and remain upright (standing or sitting) for at least 30 minutes.
Potential side effects may include:
- GERD (gastroesophageal reflux disease), heartburn
- Problem swallowing
- Nausea
- Ulcers
- Bone pain
- Joint pain
- Headaches
Denosumab (Prolia): A monoclonal antibody that helps to reduce bone breakdown (reabsorption). This medication is only given in the injection form. The medication is given every 6 months.
Potential side effects:
- Low calcium
- Muscle pain
- Joint pain
- Mild changes in cholesterol
- Skin infections
- Flu like symptoms
After your treatment with Prolia is stopped or you skip or delay taking a dose, your risk for breaking bones, including bones in your spine, is increased. Do not stop, skip or delay taking Prolia without first talking with your health care provider who can prescribe other medicines to prevent any increased risk of fractures.
Parathyroid hormone related protein: Increases bone formation. These medicines are given by the patient, a daily injection for up to 2 years and then followed by other osteoporosis medications.
- Teriparatide (Forteo)
- Abaloparatide (Tymlos)
Potential side effects:
- Dizziness when you stand up
- Headaches
- Nausea
- Low calcium
Sclerostin inhibitor: Works on both phases of bone remodeling. The major component is a decrease in reabsorption of bone, and the minor component is an increase in bone formation.
Romosozumab (Evenity) is given by 2 injections once a month in a clinic for up to a year, followed by other osteoporosis medications.
Potential side effects:
- Joint pain
- Headaches
- Muscle weakness
Estrogen (hormone-related therapy): Especially when started soon after menopause, estrogen can help maintain bone density. However, estrogen therapy can increase the risk of blood clots, endometrial cancer, breast cancer and possible heart disease.
All treatments for osteoporosis have the potential for rare but serious side effects. This does vary depending on the medication that is used for treatment. These rare but serious side effects should be discussed with your health care provider prior to starting treatment for osteoporosis.
Evaluation for Osteoporosis
If your health care provider has determined that you have osteoporosis, they may order both blood tests and urine tests to determine secondary causes (causes other than aging) of your osteoporosis. These tests can help in the selection of medication for treatment, to find out whether you are responding to treatment as expected, or to evaluate poor response to treatment. Below is a list of common tests performed in osteoporosis and does not represent all the tests that are available. Your health care provider will customize the tests ordered for you depending on your needs. Some of these tests need to be obtained when you are fasting (first thing in the morning before you have eaten).
CBC: Evaluates blood cell counts, both white cells and red cells.
CMP: Is a metabolic panel, this typically will include your kidney function, liver function, electrolytes including calcium and blood sugar.
Vitamin D level: This is a measurement of your vitamin D. Typically reported and ng/dl. An appropriate level is between 30-50 ng/dl.
24-hour urine for calcium: This is the best estimate of adequate calcium intake and absorption by the gastrointestinal tract.
Parathyroid hormone (PTH): An increase in parathyroid hormone will cause an increase loss of bone. Elevation is frequently seen in vitamin D deficiency, called secondary hyperparathyroidism.
Thyroid testing: This is to rule out you having an overactive thyroid or taking too high of dose when you are treating hypothyroidism.
Bone turnover markers: While not typically ordered for the majority of the patients with osteoporosis, these can be very helpful in certain individuals. Commonly used tests to evaluate the amount of reabsorption of bone are a urinary NTX or a serum CTX. To evaluate new bone formation, a P1NP can be obtained.
Antibodies for celiac disease: A condition that may cause poor intestinal absorption of important nutrients including calcium.
Additional x-rays of the spine may be obtained to document previous fractures. This could be with x-rays of the spine or an additional evaluation with the DXA machine called VFR (vertebral fracture recognition). Less than 70% of patients with spine fractures seek medical attention. One of the best predictors of your chance of having a fracture is a previous fracture.
Bone Density Testing
A DXA (dual energy X-ray Absorptiometry) scan is a way of measuring the amount of calcium in a bone. It’s important to have this information, because the amount of calcium in your bone contributes to how strong it is. There are multiple techniques to obtain bone density, but the most advanced is the DXA scan. These machines are located in Custer, Lead-Deadwood, Rapid City, Spearfish and Sturgis. A DXA machine uses low levels of x-ray to determine the portion of calcium in your bones.
During this painless test, you lie on a padded table as a scanner passes over your body, typically imaging your lower back and hips, occasionally a forearm. It takes only a few minutes and involves no shots, needles, or medication. In fact, you don’t even need to remove your clothes.
Who should get a DXA? ISCD (International Society for Clinical Densitometry) guidelines recommend screening post-menopausal women who have risk factors, all women after age 65, men less than 70 with risk factors, and men 70 or older.
Definition of terms that you may see on your report
Impression or diagnosis: The result of the test, typically reported in one of three categories.
- Normal: T-score -1 or greater
- Low bone mass or osteopenia: T-score between -1 to -2.5
- Osteoporosis: T-score -2.5 or less. In the US if your T-score is between -1 to -2.5 and there is an elevated FRAX score than the diagnosis will be osteoporosis
T-score: The number of standard deviations that your DXA results are different from a healthy 30-year-old population of the same sex.
Z-score: The number of standard deviations that your DXA results are different from an age-matched population of the same sex. This value is used in premenopausal women and men under the age of 50.
FRAX: Your risk of having an osteoporosis-related fracture in the next 10 years. The FRAX score is calculated using questions about age, sex, height, weight, previous fracture, parental hip fracture, current smoking, glucocorticoids (steroids) usage, rheumatoid arthritis, greater than two drinks of alcohol per day, and your femoral neck bone mineral density from your DXA test. The FRAX calculator estimates the risk of a fracture both of the hip as well as any major osteoporotic fracture for the next 10 years. An elevated FRAX score on the hip is greater than 3% and for any major osteoporotic fracture is greater than 20%.
Least significant change (LSC): LSC is the least amount of change in the bone density that can be considered statistically significant. It is determined for each DXA machine and technologist. LSC is used to determine if a patient’s DXA results have changed over time, and is used to follow bone loss as well as monitor response to treatment.
Trabecular bone score (TBS): A measure of bone texture that correlates with bone microarchitecture and strength of the bone. It can be used with the DXA result and modifies your FRAX score. It’s typically reported as normal, partially degraded, or fully degraded.
Exercising with Osteoporosis
Certain types of exercise strengthen muscles and bones, while others are designed to improve your balance which can help prevent falls. It is never too late to start exercising. Regular physical activity can increase your muscle strength, improve your balance, decrease your risk of a bone fracture, maintain or improve your posture, relieve or decrease pain. Consult your health care provider or physical therapist before starting an exercise program for osteoporosis.
The following exercises often are recommended for people with osteoporosis:
Strength training: This includes the use of free weights, resistance bands, or your own bodyweight to strengthen all major muscle groups. Spine muscles are especially important for posture. Resistance training can also help maintain bone density. Resistance training should be tailored to your ability and tolerance, especially if you have pain. A physical therapist with experience working with people with osteoporosis can help you develop a strength training routine. Proper form and technique are crucial to prevent injury and get the most from your workout.
Weight-bearing aerobic activities: These activities involve doing aerobic exercise on your feet, while your bones support your weight. Examples include walking, dancing, low impact aerobics, elliptical training machines, stair climbing, and gardening. These types of exercises work directly on the bones in your legs, hips and lower spine to slow bone loss. They also provide cardiovascular benefits. It is important that aerobic exercises are not the whole of your exercise program, as it is important to work on strength, flexibility, and balance as well. Swimming and cycling have many benefits, but they do not provide the weight-bearing load your bones need. However, if you enjoy these activities, do them. Just be sure to add weight-bearing activity.
Flexibility exercises: Moving your joints through a full range of motion will help keep your muscles working well. Stretches are best performed after your muscles are warmed up. They should be done gently and slowly without bouncing. Avoid stretches that aggressively flex and extend the spine (ie. bending at the waist).
Stability and balance exercises: Fall prevention is especially important for people with osteoporosis. Stability and balance exercises help your muscles work together in a way that keeps you more stable and less likely to fall. Simple exercises such as standing on one leg, or movement-based exercises such as tai chi or yoga, can improve your stability and balance.
Movements to avoid
High impact exercise: Activities such as jumping, running or jogging can lead to fractures and weakened bones. Avoid jerky/rapid movements in general. Choose exercises with slow, controlled movement.
Bending and twisting: Exercises in which you bend forward at the waist and twist your waist such as touching your toes or doing sit-ups can increase your risk of compression fractures in your spine if you have osteoporosis. Other activities that may require you to bend or twist forcefully at the waist are golf, tennis, bowling and some yoga poses. Some activities put you at higher risk for falls, particularly downhill skiing and horseback riding. If you are unsure how healthy your bones are, it’s best to talk to your health care provider or physical therapist about your exercise program.
Fall Prevention
The majority of fractures, secondary to osteoporosis, occur with falls. This makes fall prevention one of the most important priorities. Falls on stairs frequently result in fractures. Recommendation for stairs include 1) always have the lights turned on, 2) always use the handrail, and 3) pay extra attention when you approach the bottom of the stairs, as it is common to miss the last stair and fall. In the house, other areas with an increased risk of falls are areas that are frequently wet, including the bathroom or kitchen. In South Dakota and Wyoming, the other area of concern is outside when bad weather results in slippery surfaces. If you have to go out in bad weather, make sure you wear footwear that both stays on your feet securely and has good soles. Another potential risk for some patients involves pets. Falling over their pets or getting pulled off-balance by a pet on a leash.
Fracture Liaison Service (FLS)
Our Fracture Liaison Service, available in Rapid City and Spearfish, is specifically designed for patients who have had a fracture due to osteoporosis. It has been designed by a multidisciplinary team of health care professionals and is customized for each individual to help prevent future fractures and the associated loss of independence.